The following information provided by the American Association of Endodontics
Root Canal Treatment
Endodontic — or root canal — treatment is necessary
when the pulp, the soft tissue inside the root canal,
becomes inflamed or infected. The inflammation or
infection can have a variety of causes: deep decay,
repeated dental procedures on the tooth, or a crack or
chip in the tooth. In addition, an injury to a tooth may
cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left
untreated, it can cause pain or lead to an abscess.
Signs to look for include pain, prolonged sensitivity to
heat or cold, tenderness to touch and chewing,
discoloration of the tooth, and swelling, drainage and
tenderness in the lymph nodes as well as nearby bone
and gingival tissues. Sometimes, however, there are no
symptoms.
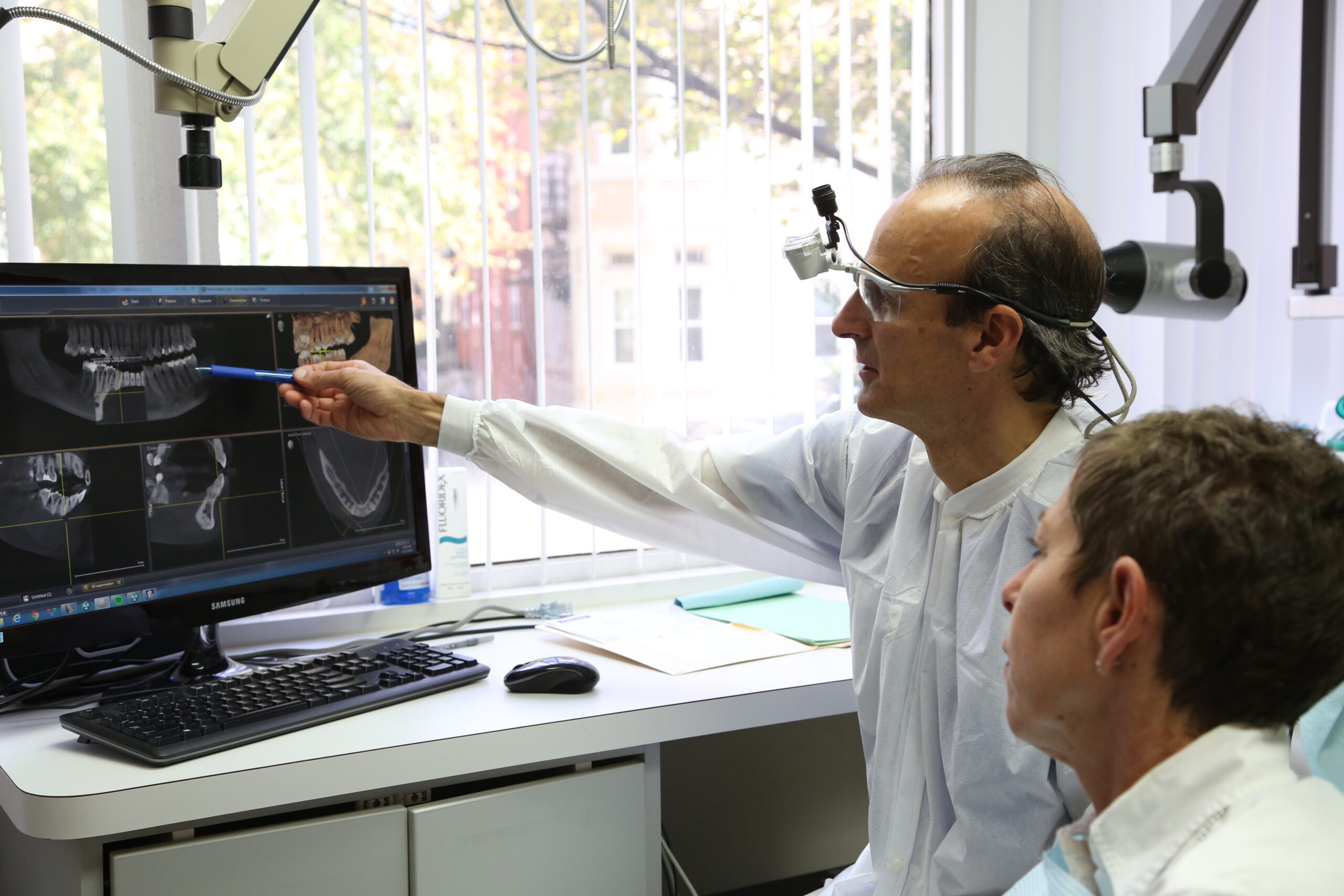
Endodontists specialize in saving natural teeth and in performing root canals.
Q & A
How does endodontic treatment save the tooth?
The endodontist removes the inflamed or infected pulp, carefully cleans and shapes the inside of the canal, a channel inside the root, then fills and seals the space. Afterwards, you will return to your dentist, who will place a crown or other restoration on the tooth to protect and restore it to full function. After restoration, the tooth continues to function like any other tooth.
Endodontic Procedure
Endodontic treatment can often be performed in one or two visits and involves the following steps:
1. The endodontist examines and x-rays the tooth, then administers local anesthetic. After the tooth is numb, the endodontist places a small protective sheet called a “dental dam” over the area to isolate the tooth and keep it clean and free of saliva during the procedure.
2. The endodontist makes an opening in the crown of the tooth. Very small instruments are used to clean the pulp from the pulp chamber and root canals and to shape the space for filling.
3. After the space is cleaned and shaped, the endodontist fills the root canals with a biocompatible
material, usually a rubber-like material called “gutta-percha.” The gutta-percha is placed with an adhesive cement to ensure complete sealing of the root canals. In most cases, a temporary filling is placed to close the opening. The temporary filling will be removed by your dentist before the tooth is restored.

4. After the final visit with your endodontist, you must return to your dentist to have a crown or other restoration placed on the tooth to protect and restore it to full function.

If the tooth lacks sufficient structure to hold the restoration in place, your dentist or endodontist may
place a post inside the tooth. Ask your dentist or endodontist for more details about the specific
restoration planned for your tooth.
Will the tooth need any special care or additional treatment after
endodontic treatment?
You should not chew or bite on the treated tooth until you have had it restored by your dentist. The
unrestored tooth is susceptible to fracture, so you should see your dentist for a full restoration as soon as possible. Otherwise, you need only practice good oral hygiene, including brushing, flossing, and regular checkups and cleanings.
Most endodontically treated teeth last as long as other natural teeth. In a few cases, a tooth that has undergone endodontic treatment does not heal or the pain continues. Occasionally, the tooth may become painful or diseased months or even years after successful treatment. Often when this occurs, redoing the endodontic procedure can save the tooth.
What causes an endodontically treated tooth to need additional treatment?
New trauma, deep decay, or a loose, cracked or broken filling can cause new infection in your tooth. In some cases, the endodontist may discover additional very narrow or curved canals that could not be treated during the initial procedure.
Why do I need another endodontic procedure?
As occasionally happens with any dental or medical procedure, a tooth may not heal as expected after initial treatment for a variety of reasons:
Narrow or curved canals were not treated during the initial procedure.

Complicated canal anatomy went undetected in the first procedure.
The placement of the crown or other restoration was delayed following the endodontic treatment.
The restoration did not prevent salivary contamination to the inside of the tooth.
In other cases, a new problem can jeopardize a tooth that was successfully treated.
For example: New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth.

A loose, cracked or broken crown or filling can expose the tooth to new infection.
A tooth sustains a fracture.
What will happen during retreatment?
First, the endodontist will discuss your treatment options. If you and your endodontist choose retreatment, the endodontist will reopen your tooth to gain access to the root canal filling material. In many cases, complex restorative materials—crown, post and core material—must be disassembled and removed to permit access to the root canals.

After removing the canal filling, the endodontist can clean the canals and carefully examine the inside of your tooth using magnification and illumination, searching for any additional canals or unusual anatomy that requires treatment.

After cleaning the canals, the endodontist will fill and seal the canals and place a temporary filling in the tooth. If the canals are unusually narrow or blocked, your endodontist may recommend endodontic surgery. This surgery involves making an incision to allow the other end of the root to be sealed.

After your endodontist completes retreatment, you will need to return to your dentist as soon as possible to have a new crown or other restoration placed on the tooth to protect and restore it to its full function.

What are the alternatives to retreatment?
If nonsurgical retreatment is not an option, then endodontic surgery should be considered. This surgery involves making an incision to allow access to the tip of the root. Endodontic surgery may also be recommended in conjunction with retreatment or as an alternative. Your endodontist will discuss your options and recommend appropriate treatment.
What are the alternatives to endodontic retreatment and/or endodontic surgery?
The only other alternative is extraction of the tooth. The extracted tooth must then be replaced with an implant, bridge or removable partial denture to restore chewing function and to prevent adjacent teeth from shifting. Because these options require extensive surgery or dental procedures on adjacent healthy teeth, they can be far more costly and time consuming than retreatment and restoration of the natural tooth.
No matter how effective tooth replacements are—nothing is as good as your own natural tooth. You’ve already made an investment in saving your tooth. The payoff for choosing retreatment could be a healthy, functioning natural tooth for many years to come.
Copyright © 1995-2011 American Association of Endodontists (AAE), All Rights Reserved